100+ coronavirus questions answered by doctors - KSDK.com
100+ coronavirus questions answered by doctors - KSDK.com |
| 100+ coronavirus questions answered by doctors - KSDK.com Posted: 29 Apr 2020 05:57 PM PDT We are taking some of your questions straight to the Washington University Infectious Disease physicians at Barnes-Jewish Hospital ST. LOUIS — Concerns over the coronavirus, officially named COVID-19, have led to major changes across the St. Louis area. 5 On Your Side is focusing on giving you facts and not spreading fear. So, we are taking some of your questions straight to the Washington University Infectious Disease physicians at Barnes-Jewish Hospital. They addressed some of the top local questions people have and also discussed how concerned St. Louisans should be. You can read their responses below. If you have a question, you can text us at 314-444-5125. And follow our latest coronavirus coverage at KSDK.com/coronavirus and on the 5 On Your Side app. Since there are so many questions in this story, try using Ctrl+F on your desktop to search keywords of the answers you're looking for. On your cell phone, there should be an option to search for words on this page as well.
Coronavirus resources:
Is it too early for grandparents to start babysitting again?It is likely that COVID-19 will be around for some time and we still need to take precautions against it. As the community relaxes some precautions, it will be important that you continue to follow the recent habits you've developed, including washing your hands, social distancing, coughing into your elbow and staying away from people if you are feeling ill. You should not be around people who are ill, which includes children.
The WHO said there is no evidence that getting COVID once insures immunity. How will the medical community determine if immunity is conferred by being infected with COVID?We are developing tests to determine if people have developed antibodies after recovering from COVID-19. There is still a lot that is unknown about this virus, including what particular antibodies make a person immune to infection and, if you have been infected, how long immunity lasts. Those questions are being actively studied.
I am hearing obesity is an underlying condition by itself with COVID, especially for younger people. Is that true?Yes, obesity, like lung disease and diabetes, is a risk factor for having a more severe illness with COVID-19.
The public was initially told not to wear a mask and now is being told — and in some cases required — to wear a mask, why the change?Based on what we knew about the infections caused by two other novel coronaviruses, SARS and MERS, it was not thought that wearing a mask would have a significant impact on spread of the virus. A person only starts to spread those viruses once they develop symptoms. As we learned more about the virus causing COVID-19, we found that some people who are infected do not have symptoms. Also, some people may spread the virus before they develop symptoms. Given that new knowledge, wearing a mask in public will prevent people from unwittingly spreading the virus to other around them.
Couldn't the stats be skewed by the fact that everyone's self-quarantining because of COVID-19? Then, of course, the flu numbers will be down. What were they last year at this time?We have seen good evidence that the social distancing measures in the St. Louis region have slowed the spread of COVID-19 and influenza. Influenza numbers start to decrease in the spring every year, but this year they dropped more rapidly than usual.
I've been taking hydroxychloroquine for 10 years. Could my risk of contracting COVID-19 be lower because of this?We do not know yet if hydroxychloroquine is effective at either preventing or treating COVID-19. There are clinical trials underway right now that should give us the answer to these questions in the coming weeks.
Once the U.S. is reopened, how are we to maintain and remain healthy when there might still be a shortage of hand sanitizer, sanitizer wipes and sprays?The most important thing we can do to remain healthy now is to avoid close contact with people who don't live with us and to wash our hands frequently. While hand sanitizer is effective at cleaning our hands, plain old soap and water work, too. As the social distancing measures are slowly relaxed it will still be important to avoid contact with people who could be infected, wash our hands frequently and clean frequently touched surfaces.
Our extended family has a shared home at the Lake of the Ozarks. Is it safe for each of our families to take turns visiting on different weekends?Social distancing and shelter orders aren't only to protect yourself from the virus. They are also there to reduce the burden on healthcare and public services in the face of a surge of sick patients. During this time, all vacations and outings should be limited to only what is necessary. It is important that everyone, including those who are not sick, do their part to reduce the spread of infection and any potential burden on the healthcare system by staying at home as much as possible.
A New York newspaper ran an article saying that a product undergoing FDA trials to treat herpes, TML, from Beech Tree Labs "reverses COVID-19." Is there any evidence that this substance (described as microdose thimerosal) has been tested on COVID-19 or any indication that it would be effective? Is anything like it being tested by the FDA for effectiveness?Be wary of any product that claims it can "beat COVID". Finding effective therapies should be a rigorous and thorough process. Several medications and chemicals have been shown to be effective at reducing viral replication in the lab. However, many of these have failed to show any benefit in actual human studies.
Does the pneumonia vaccine offer any protection that would make someone less likely to get COVID-19 or less likely to have pneumonia if they do get COVID-19?The pneumococcal (pneumonia) vaccine helps to protects against a particular bacterium called Streptococcus pneumoniae. It has no effect on preventing COVID-19.
Once a ventilator has been used, can it be sanitized and have parts replaced to be reused? Does every ventilator have to be new?Ventilators undergo cleaning and disinfection in between patients.
If a person is admitted to the hospital for chest pains, does the CDC say that patient should be included in the COVID-19 count?If the person is tested for COVID-19 and the results return positive, that information will be relayed to the appropriate health authorities. A physician will make the determination of whether further workup or testing is indicated after reviewing the clinical history.
Can excessive strenuous exercise, such as distance running, suppress the immune system, leaving a person more susceptible to COVID-19?There is still a lot we do not know about the virus. We do know that people with certain medical conditions, such as chronic heart and lung disease, are more at risk for severe illness. This specific circumstance has not been studied. However, to avoid becoming ill with the disease, we recommend following guidance provided by local and federal authorities that include social distancing and hand hygiene.
My doctor had a patient who ended up being admitted to the hospital for COVID-19. I was the next patient the doctor saw after that. Should I be concerned?You should discuss your specific situation with your doctor. Regardless, it is a good idea to monitor yourself for symptoms of COVID-19 and immediately report any new concerns to your doctor.
How is nitric oxide used to treat severe COVID-19 patients?Nitric oxide is being explored as a potential therapy for patients with severely damaged lungs (a condition known as acute respiratory distress syndrome or ARDS). Nitric oxide, when delivered by inhalation to patients on a ventilator, acts to improve blood flow in certain areas of the lungs to increase the amount of oxygen in the bloodstream. Nitric oxide has other effects on the heart and vascular system. Previous studies evaluating the effect of nitric oxide in patients with SARS (or Severe Acute Respiratory Syndrome) showed possible benefit. Little is known about the effect of nitric oxide in COVID-19. Additional studies are needed before this is used in the routine care of patients with COVID-19.
Can COVID-19 droplets be transmitted through the shared ventilation system in an apartment complex?The spread of coronaviruses from person-to-person over long distances, such as through HVAC systems, has not been shown.
Is it possible we are making resistant "bugs" with all the wiping down with antiseptic?There is no evidence that the coronavirus has developed resistance similar to what we see with bacteria. Traditional antiseptics, like alcohol and soap, act in a way that does not typically allow resistance to develop in any organism, including viruses.
I'm 65 and have high blood pressure. Will I ever be able to go back to a normal life until there is a vaccine or a medication available?The coronavirus pandemic will likely cause a long-term change in behavior going forward, even after the "peak" outbreak has passed. Even after the attention subsides, the habits we developed, including washing your hands and appropriate social distancing, should carry forward at a reasonable level to protect ourselves and those around us from this virus and other similar infections.
Since COVID-19 causes oxygen deprivation, why aren't patients given hyperbaric chamber treatments?Clinical trials are underway to see if this is an effective treatment for COVID-19, but we have no data to show if it is effective.
I regularly receive mail from Europe. I'm not worried about the envelopes, but rather the items sealed inside. Should I worry about opening those sealed items exposing what's inside to the air for the first time since they were packaged?The chances of catching the virus from a sealed package in the mail is likely very low. While the virus can survive on many surfaces for several hours to several days, the most important way to get infected is through respiratory droplets and close contact with an infected individual. It is important to always wash your hands immediately after handling any delivered items.
During windy days, can I get COVID-19 if I'm sitting in the backyard with no mask on?If you are sitting by yourself outdoors with no other person nearby there is no known risk of getting COVID-19 and you would be safe without wearing a mask. The most important thing to protect yourself is to keep your distance from others whenever possible.
How are people supposed to know if they are completely rid of COVID-19 after 14 days if they aren't retested?Even with re-testing, we cannot know for certain exactly when people get rid of the virus because the tests can sometimes be falsely positive or falsely negative. If you have had COVID-19, you should consider yourself to be contagious until at least seven days have passed since you first felt sick, and you have been without any symptoms for at least three days. Those whose symptoms have resolved and 14 days have passed are thought to be much less likely to spread the virus to somebody else.
Why is it OK to eat food prepared by others during the COVID-19 pandemic? Isn't that unnecessarily risking further exposure?Currently there is no evidence of food or food packaging being associated with transmission of COVID-19. We advise that anyone who prepares food (or has any other job) talk to their supervisor if they have symptoms of fever, cough or shortness of breath, or if they have had recent exposure to another person diagnosed with COVID-19 to determine if they should continue to work.
Why can't swab testing be effective in the mouth or throat? What happens to the swab and sample in the lab?Swabs from the mouth can detect the virus that causes COVID-19, but it is not quite as accurate as the swabs deep in the nose. Several laboratories are working on a quick swab test to determine if you have the virus or not. So far none of the over-the-counter or at-home mouth swab test kits are accurate enough to be used.
What is the most sanitary way to pay for groceries or at a drive-thru? Cash or credit cards?It is not certain that one way is safer than the other. Some data suggest that coronaviruses may persist for hours to several days depending on the type of surface, temperature or humidity of the environment. This is why it is important to always wash your hands when handling materials such as money that may have come into contact with the virus.
It has been mentioned that diabetes is an underlying condition. Does that include both Type 1 and Type 2?In general, we don't know of any reason to think COVID-19 will pose a difference in risk between Type 1 and Type 2 diabetes. People who already have diabetes-related health problems are likely to have worse outcomes if they contract COVID-19 than people with diabetes who are otherwise healthy, whichever type of diabetes they have.
Are the flu and COVID-19 in any way related?Influenza virus and SARS-Coronavirus-2 (the virus that causes the disease COVID-19) are not genetically related, they come from different virus families. However, both viruses cause respiratory illnesses that can be severe in some people and are passed from person to person.
If a person has tested positive for COVID-19 but is now symptom-free, is it safe to say that person is out of danger?According to the CDC, patients who have tested positive and are no longer symptomatic should stay in isolation for seven days after symptom onset or 72 hours after resolution of symptoms, whichever is longer, to ensure that they are no longer infectious. More data is being released to show that we have immunity after contracting the coronavirus once. However, we still do not have enough information to say for certain how long that immunity lasts.
Something I saw online said Purell is antibacterial, but COVID-19 is a virus. Is Purell an effective preventative?A lot of the same properties that make soaps antibacterial also make them antiviral. This includes antibacterial soaps and hand sanitizers like Purell that have alcohol content of at least 60%.
Are people with lupus who take hydroxychloroquine less likely to contract COVID-19?We do not have any data to say that hydroxychloroquine is effective at preventing infection with COVID-19. However, those studies are ongoing.
Can COVID-19 last longer on refrigerated or frozen surfaces?In general, coronaviruses can live on most surfaces for hours to days, depending on temperature, humidity and the kinds of surfaces. The virus can live a little longer in cooler temperatures, though there is believed to be very low risk of spread from food products or packaging that are shipped over a period of days or weeks at ambient, refrigerated or frozen temperatures.
My daughter was told by a scientist that people with O positive blood cannot contract COVID-19. Is this true?One study showed patients with Type O blood were slightly less likely to contract COVID than other blood types, but were not, by any means, immune to the disease. Everybody, regardless of blood type, should do their best to avoid catching the virus or spreading it to others by maintaining social distancing, washing hands frequently and staying home, especially if you feel ill.
If I go outside to take a walk in my neighborhood, do I need to wear a face mask?The most important part of social distancing is avoiding being within 6 feet of people who don't live with you. The CDC recommends wearing a cloth face covering or face mask when outside of your home if you cannot avoid being within 6 feet of others (such as in grocery stores). If you can't avoid being this close to people on your walk, then a cloth face covering or mask should be worn.
If I wear a fabric mask, does it help to put it in a Ziploc bag and microwave it for 2-3 minutes to sanitize?Microwaving masks could be dangerous and a risk for fire depending on what materials are used. It might also potentially damage the mask, reducing its effectiveness. Fabric masks should be made of a material that can be washed in the laundry.
Our neighbor's dog frequently sneaks into our backyard to play with our dog. Could he potentially pass COVID-19 to us?We do not know to what extent transmission between dogs and other animals can occur. At this time, there is no known risk of catching COVID-19 from pets. Regardless, it is important to wash your hands frequently.
So, if we suspect people who are asymptomatic are spreading the virus, why isn't everyone being tested; why just those with symptoms?While the ability to test people for COVID-19 has improved in the last month, there is still limited availability of testing supplies in the United States. It is true that people can pass the virus shortly before they become symptomatic. It is for that reason that we continue to stress the importance of social distancing and appropriate hand hygiene at all times. That is the single best way that you can protect yourself and those around you from the virus.
Since hand soap kills germ on your hands does it work on household surfaces as well?Soap and water are important to use on surfaces if they are visibly dirty, since disinfectants will not work as well if a surface is dirty. The CDC does recommend using disinfectants on surfaces, especially high-touch surfaces like light switches and door handles.
We see areas being sprayed for the virus. Why can't that be done to masks and/or other PPE for reuse?Antiviral sprays may damage the mask. Also, wet masks do not work as well as a barrier.
Can I microwave a homemade mask to sanitize it? Does CPAP ozone cleaner work on a homemade mask?Microwaving masks can be dangerous. Microwaving can damage and melt the material, reducing its effectiveness. Additionally, exposing cloth and non-microwave safe materials to a microwave is a probable fire hazard.
How long is a wipe effective? Should I use one wipe per item?Wipes should be used according to the manufacturer's instructions. Enough wipes should be used for the treated surface to remain visibly wet for a specified amount of time.
If a homemade mask helps protect others from me, why wouldn't it help protect me from others?Masks protect others from a potentially asymptomatic person or someone with minor symptoms who is shedding the virus. But they may also act as a barrier to protect a person from respiratory droplets from others (which is how COVID-19 is thought to primarily spread). Masks should be used with all the other practices we've been mentioning: frequent hand washing, avoid touching eyes, nose and mouth and continue to practice social distancing. These practices will help you avoid infection.
Some experts are already talking about another wave of COVID-19 in the fall. Is it really necessary to worry about that already?Little is known about the future of the current COVID-19 pandemic and if the virus will return in the fall. It is possible, but we do not have enough information since this is a new virus.
Does spraying masks with antibacterial spray increase their safety? Does doubling up of masks increase effectiveness?Antibacterial sprays should not be used on masks as they are not effective against viral infections (such as the one that causes COVID-19) and may degrade the quality of the mask. Wearing two masks at the same time is not recommended.
Are swimming pools safe? Will the chlorine in the pools kill COVID-19?Limited data is available about swimming pools. We would recommend following guidance from local and federal public health officials. As always, people with gastrointestinal symptoms should not use swimming pools, and you should practice social distancing.
Is there a link between pink eye and COVID-19?Pink eye is an infection characterized by redness, swelling and tearing of one or both eyes. Pink eye is usually caused by bacteria and viruses that are distinct (or different) from the virus that causes COVID-19. Some early research has shown that very rarely patients with COVID-19 may experience symptoms similar to pink eye. However, patients with COVID-19 usually have other symptoms that are not present with pink eye including shortness of breath and cough.
My neighbor left me freshly-baked cookies in a plastic bag. Is it safe to eat them?Infection is unlikely to occur in this way. We know that infection occurs through close contact with others who are ill, specifically through contact with respiratory droplets. Infection may also spread through contact with contaminated surfaces as well. We recommend frequently washing your hands, especially after contact with food containers and packaging in order to minimize the chances of acquiring infection.
Is there any way to know or find out if you have had a mild case of COVID-19 and have recovered from it?There are some antibody tests which are being developed to see if a person has antibodies from the virus that causes COVID-19. One fingerstick test was approved by the FDA just this week but is not yet widely available. Beware of companies claiming to have at-home testing, since there are no tests approved for home testing at this time.
Being a severe asthmatic, how can I tell the difference between my asthma and COVID-19?It can be difficult to determine the difference between your asthma and COVID-19 infection because the same symptoms can occur in both. However, we recommend that you be aware of your usual asthma symptoms and monitor for any worsening. Understand what your asthma triggers are and if you notice any worsening from your usual symptoms or start to develop fevers, then you should contact your primary care provider.
My spouse and I are both at risk. How should we proceed if one of us gets ill with COVID-19 so as to NOT transmit it to our spouse?Have the sick person stay in a room away from other people as much as possible. If possible, have them use a separate bathroom, avoid sharing household items. If facemasks are available, the sick individual and healthy individual should wear them when around each other. Wash your hands often. Avoid touching your eyes, nose and mouth. Every day, clean frequently touched surfaces. Avoid having any other visitors. If laundry is soiled, when washing wear disposable gloves and keep soiled items away from your body. Wash your hands as soon as gloves are removed.
Is it true you can microwave your mail to kill COVID-19?It is not necessary to use a microwave to sterilize everyday items that have a low risk of having any contact with the virus. There is no study to show the effectiveness of using a microwave to kill the virus. It is best to wash your hands after you have contact with any object or parcel you are concerned may have had contact with COVID-19.
Can wearing a respirator mask increase the oxygen level of a person with severe COPD? What mask would you recommend to someone with COPD?Respirators do not increase the oxygen level, they protect individuals from inhaling very small particles with potential infectious organisms. People in the community do not need to wear respirators or masks even if they have underlying medical conditions such as COPD, unless they develop symptoms concerning for COVID-19, in which case a surgical or isolation mask would suffice. The best way to protect yourself is to practice social distancing, wash your hands frequently with soap and water or alcohol-base hand sanitizer and avoid touching your face.
Does COVID-19 live in your throat for four days before moving into your lungs? Will drinking hot beverages or water keep the virus from staying there?This is false. The incubation period (the time it takes for symptoms to develop) is thought to be between 2-14 days, but most commonly symptoms seem to emerge around 5 days. It is incorrect to suggest that people could cure themselves by gargling or drinking hot beverages during this time. Although the virus is transmitted via respiratory secretions, there is no evidence that the virus remains in the throat and that gargling or drinking hot beverages will help eliminate the virus. There is a lot of misinformation concerning COVID-19, mostly coming from social media. Make sure you can fact check any information with verified sources such as CDC or WHO.
If you've stayed at home for 14 days and your family (who lives close by) has also stayed at home for 14 days with no symptoms, can you visit each other?Continuing social distancing is the best way to protect yourself and others from getting sick, especially given the increasing number of cases and risk of transmission in the community.
If you are currently taking Plaquenil (hydroxychloroquine), does it help prevent you from getting COVID-19, or does it make you less responsive to the medication if you get the virus?At this time, we still do not know if hydroxychloroquine if an effective medication to treat or prevent COVID-19. There are many clinical trials around the world and the U.S. trying to answer this question.
If I go grocery shopping, should I change my clothes and take a shower when I get home?There is no recommendation that you need to change your clothes or take a shower after grocery shopping. Necessary steps to protect yourself would include washing your hands after being in a public place and avoid touching your eyes, nose and mouth with unwashed hands.
How is the waste from hospitals being disposed of, and is the COVID-19 virus carried in that waste?The CDC's FAQ page addresses waste management. "Waste generated in the care of patients with confirmed COVID-19 does not present additional considerations for wastewater disinfection in the US. Coronaviruses are susceptible to the same disinfection conditions in community and healthcare settings as other viruses, so current disinfection conditions in wastewater treatment facilities are expected to be sufficient. Medical waste (trash) from healthcare facilities treating COVID-19 patients is no different than waste coming from facilities without COVID-19 patients. Management of medical waste should be performed in accordance with routine procedures. There is no evidence of suggest that facility waste needs any additional disinfection." SARS-CoV-2 (or the virus that causes COVID-19) has been detected in stool specimens from patients with COVID-19. It remains unclear if someone can contract COVID-19 through contact with waste products. Avoid contact with waste products. If this cannot be avoided, perform hand hygiene afterwards.
I have an 18-year-old who just doesn't get it. He stays in for a few days, then says he wants to take a walk and ends up with a friend riding in cars. He doesn't look at the news, so he's clueless. Is there anything I can do or say to reach him? I'm afraid for my life and my other children. Articles maybe? I'm overwhelmed with anxiety for us all.The article and video below are aimed specifically at younger people to explain the importance of COVID-19. The video brings up a good point that although a young person may feel well and/or experience mild symptoms after contracting illness, there is still a risk of them transmitting the virus to someone who is at risk of becoming very sick if they get infected. Additionally, more recent studies have shown that even though young people are at less risk of severe disease and death than individuals over age 60, some young people do get very sick and can die from it.
I've seen this floating around on social media. Is it true?Doctors are reporting they now understand the behavior of the COVID-19 virus due to autopsies that they have carried out. This virus is characterized by obstructing respiratory pathways with thick mucus that solidifies and blocks the airways and lungs. So, they have discovered that in order to apply a medicine you have to open and unblock these airways so that the treatment can be used to take effect. However, all of this takes a number of days. Information from social media can oftentimes be misleading. The majority of patients who have COVID-19 experience very mild symptoms and no specific interventions are recommended besides rest and use of over-the-counter medications. Some patients with severe illness who are on ventilators can develop mucus obstruction of the airways, just like what can happen with other respiratory infections. When this happens, ICU doctors and nurses recognize it and can treat it. This is not something that can be done at home.
Can organs from a donor who had COVID-19 be used for transplants?Because of the possibility of passing COVID-19 to the organ recipient, organs from patients with COVID-19 cannot be used for transplants.
Is there data that show people with better lung capacity (e.g., runners, swimmers, bicyclists) fare better if exposed to COVID-19?Data has shown that high-risk populations (people over age 60 and those with underlying medical conditions, such as chronic heart and lung disease and diabetes) are more likely to progress to severe disease after exposure to COVID-19 than younger people without underlying medical problems. It is not known if athletes would have better outcomes from COVID-19.
Can mosquitoes carry COVID-19 by biting an infected person and then biting someone else?There is no evidence that it is transmitted through mosquitoes. The primary form of transmission is through droplets generated when infected people cough or sneeze or through droplets of discharge from the nose. To prevent the spread of the infection, frequently wash hands thoroughly and avoid close contact with anyone who is coughing or sneezing.
Are older CPAP machines of any use to medical facilities as ventilators during the COVID-19 pandemic?CPAP machines are useful for the treatment of conditions such as obstructive sleep apnea; however, they are not a substitute for ventilators that are needed to treat people with severe COVID-19 infection.
I believe I had COVID-19 in January. How can I get my plasma tested for antibodies, and is it worth doing?Antibody tests to determine if you have been previously infected are not yet commercially available, but they are in development. We do not know yet if prior infection will lead to long-lasting protection against future infection, but if that turns out to be true, then it may become important in the future for people to know their status.
I am a 64-year-old woman who had pneumonia four years ago that caused heart failure. I am healthy now. Am I at a lower risk of contracting COVID-19 if I have had both pneumonia shots?The pneumonia shots, Pneumovax and Prevnar, are vaccines that help protect patients against pneumonia caused by certain bacteria. It does not provide any protection against viral infections such as COVID-19.
I have Multiple Sclerosis, which causes body aches all the time and fatigue — sometimes even an elevated body temp like 99.9. I also have chills and shortness of breath. How do I know the difference if I was to contract COVID-19?The key is to note any symptoms that are outside of normal for you. If you develop any new or worsening symptoms you should discuss with your primary care provider to decide the next steps. The main symptoms of COVID-19 are cough, shortness of breath and fever. However, additional symptoms could include any, or none, of the following: loss of sense of taste and smell, fatigue, muscle aches, sore throat, headache or diarrhea.
I have a relative who is sick with a fever between 101-104, and she can't be tested until April 1. What is she supposed to do until then? What if her breathing gets worse?Any person with fever, cough or shortness of breath should be aware that these symptoms could be from COVID-19. Any person with these symptoms should discuss with their primary care provider to decide the next steps. While waiting for testing, it is advisable to stay at home in self-isolation (see link here). Any person who begins to develop worsening symptoms, including new chest pain not related to cough, worsening shortness of breath, confusion, bluish discoloration to the lips or coughing up blood should seek immediate medical attention.
How can anyone say that the COVID-19 pandemic is "leveling off" when people haven't been tested?At this time, there is no evidence that the numbers of people testing positive for COVID-19 is leveling off. In fact, the pandemic is continuing to accelerate quickly across most of the country. On Thursday, the United States became the country with the highest number of confirmed COVID-19 cases.
We are not supposed to touch our eyes. Could you explain why? I wear contact lenses and I put them in every morning and take them out every night. I wash my hands thoroughly several times a day.We know that infection occurs through close contact with respiratory droplets from others who are ill. We also know that infection may occur through contact with contaminated surfaces. When a person touches their face (and their eyes) after coming into contact with the virus, there is a chance of developing illness. Thus, we would recommend washing hands frequently throughout the day. This includes washing hands prior to putting contacts in and taking them out.
Can a person be infected again with COVID-19 after recovering?There were some early reports in Japan and China of people becoming re-infected with COVID-19, but there is not enough data to see if this is really the case. Once a person recovers from illness, there is evidence that some immunity to the virus forms. It remains unclear if this immunity grants full protection from infection after re-exposure.
What is the risk of getting COVID-19 from ordering take-out food or going through a drive-thru? Should these be avoided and used only as a last resort?Infection is unlikely to occur in this way. We know that infection occurs through close contact with others who are ill, specifically through contact with respiratory droplets. Infection may also spread through contact with contaminated surfaces as well. We recommend frequently washing your hands, especially after contact with food containers and packaging in order to minimize the chances of acquiring infection.
Is it necessary for a senior living alone to continually wash and sanitize hands?To protect yourself, it is recommended that you clean frequently touched surfaces and frequently wash your hands throughout the day especially after you have been in a public place, after blowing your nose, coughing or sneezing.
At what point or stage is COVID-19 detectable? Does a person have to wait for symptoms? It seems waiting that long is not the best thing for the public.With the tests currently available, it may be possible to detect the virus up to 48 hours before a person begins to develop symptoms. The problem is that testing an asymptomatic person today does not mean that they will not develop infection later. It is important to test who is the most at risk of infection. If you develop symptoms of cough, fever or shortness of breath, talk to your doctor and follow their instructions on self-quarantine or seeking further medical attention. It is also very important that you always wash your hands and maintain social distancing whenever possible.With so much news coverage devoted to COVID-19, what is the effect on someone's mental health? Everyone reacts differently to stressful situations, with fear and worry about yourself and those around you. People can have changes to their eating patterns, difficulty sleeping and feelings of fear, anxiety and depression. It is a stressful time, don't forget to support yourself in a healthy manner. Take breaks from following stories about the pandemic, take care of your body with exercise, stretches or meditation. Try to eat healthy, well balanced meals and talk to others who you trust about how you are feeling. Here are a couple of key numbers that should be available to anyone that needs help.
If a person passes away from COVID-19, can their body still carry the disease and potentially infect other people?According to the CDC, It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose or possibly their eyes, but this is not thought to be the main way the virus spreads. People should consider not touching the body of someone who has recently died of COVID-19. Older people and people of all ages with severe underlying health conditions are at higher risk of developing serious COVID-19 illness. There may be less of a chance of the virus spreading from certain types of touching, such as holding the hand or hugging after the body has been prepared for viewing. Other activities, such as kissing, washing and shrouding should be avoided before, during and after the body has been prepared, if possible. If washing the body or shrouding are important religious or cultural practices, families are encouraged to work with their community cultural and religious leaders and funeral home staff on how to reduce their exposure as much as possible.
Should we practice social distancing with our spouse or significant other?If you have any symptoms, you should certainly try to stay away from others in the home, even so far as to have a designated "sick room" away from others in the home with use of a separate bathroom, if available. If you are both asymptomatic and you have had no exposure to someone else who is sick, you should do all of the things we mention to reduce the risk of spread of potential infection: try avoid sharing utensils, wash your hands, clean surfaces regularly and cough into your elbow.
As a person who cleans homes for a living, is it safe for me to still clean them? No one else is inside the home when I'm there.Talk with your employer to see if you should receive specific training on limiting the spread of illness and providing increased attention to high touch surfaces in the home. To protect yourself, consider calling ahead to see if your customers are having any symptoms such as fevers, cough or shortness of breath which could put you at risk. The virus can be present on surfaces for several days. Protect yourself with frequent hand washing, use gloves and avoid touching your face if at all possible.
How do you shop for and clean fresh produce during the coronavirus outbreak? Do we really have to wipe down boxes, packages and food from the grocery store with a bleach solution?There is currently no evidence to suggest that COVID-19 can be transmitted through food or water systems, but sharing food and beverages is discouraged to reduce the risk of sharing saliva. Proper home food safety is advised, including promptly refrigerating foods, keeping raw and cooked foods separate, rinsing fresh produce and heating food to the appropriate internal temperature. While it is OK to wipe down some packages you get from the store, the most important step to remember is to always wash your hands after handling packages and avoid touching your face.
Is it safer to breathe through your nose instead of through your mouth when in public places?The virus is spread through respiratory droplets from infected people. If you are in close contact (fewer than 6 feet) from a sick person who is coughing or sneezing, these droplets can be inhaled through your nose or mouth. Breathing through your nose or mouth will not make a difference. You should avoid public places and distance yourself from others.
Are people living with HIV or AIDS who are already on antiviral drugs less at risk for contracting COVID-19?HIV treatment (or antiretroviral therapy) involves antivirals targeted against human immunodeficiency virus. There is no evidence that people living with HIV on antiretroviral therapy will have a lower likelihood of acquiring COVID-19 and the use of these medications should not be encouraged as treatment or prophylaxis for COVID-19. There was some thought that one particular HIV drug (Kaletra) might be effective against COVID-19 but the early research indicates it probably does not have any benefit in preventing or treating COVID-19.
Does COVID-19 thrive in cold temperatures? Should I keep my house warmer than usual?The most effective way to protect yourself from COVID-19 is with frequent handwashing with soap and water or using hand sanitizer and social distancing. We really don't know whether or not there will be a seasonal component to this. At this time, we assume that COVID-19 can be transmitted anywhere, regardless of how hot or humid the air is.
Is hand sanitizer still effective if it's expired?Sanitizer past its expiration date may still have some effectiveness, because it still contains alcohol which is the active ingredient. Try to use hand sanitizer that contains at least 60% alcohol.
I live alone, go out to the deck in my building to walk once a day and wash my hands like I should. Do I need to sanitize apartment daily (e.g, wipe down things)?You should try to sanitize "high-touch" surfaces or places which you frequently touch. Frequent hand hygiene and distancing yourself from others are also important strategies that you should continue practicing regularly.
People all over Facebook are asking craft people to make and donate masks for hospitals. Is a homemade mask protective for medical professionals?Given the recent shortage of personal protective equipment for healthcare professionals, the CDC has indicated that homemade masks (banda, scarfs) can be considered for use by healthcare practitioners as a last resort when proper facemasks are not available. Homemade masks are not considered protective equipment since their capacity to protect is unknown. Caution should be exercised when considering this option. They should be used in combination with a face shield that covers the entire front and sides of the face.
I recently moved into a new apartment and this weekend wanted to have a few family members over for dinner, maybe 6 to 8 of us. Is this okay? And also, what if your family you're staying with is big, say 10 or more? What are the recommendations for large families?It is recommended to continue with social distancing strategies and frequent hand hygiene to avoid any possible community spread. You should consider postponing any non-essential meetings including large family gatherings. Another option would be to have virtual meetings. When smaller gatherings must occur, make sure nobody is sick with fever, cough or shortness of breath and that nobody has had recent contact with a COVID-19 patient.
Since this is a respiratory virus, will we see an exponential increase with those who are vaping?People with underlying pulmonary disease are at risk of developing severe illness from COVID-19. Smoking or vaping might compromise the ability of the upper airways to clear bacteria and viruses in general. However, there are no studies available regarding COVID-19 in this group.
I was wondering if it's safe to use my own reusable bags when I go grocery shopping? Or should I use the plastic ones provided by the store? If I do use my own, should I disinfect them when I bring them home?It is safe to use reusable bags and clean them as you normally would. Also remember to practice frequent hand hygiene.
Is it safe to consume fresh produce that is not wrapped and has been handled by customers?There is no reason to fear consuming fresh produce.
Is there new guidance about not taking ibuprofen to treat COVID-19?There is no scientific data on the harms of ibuprofen in treating COVID-19. Until there is more firm evidence, the World Health Organization recommends avoiding ibuprofen and considering acetaminophen instead. Again, there is no firm data to show harm, but until there is, it is recommended that ibuprofen be avoided. Acetaminophen should be taken as per medication instructions, and you should ask your doctor if you have any specific concerns about taking this drug that are related to other medical issues.
I keep reading that if you have Type A blood then you are more likely to be susceptible to getting the coronavirus. Is this true?According to one study published from Wuhan, China, people with certain blood types were more likely to have the infection. The increased chance for infection was small. Since it is only one study, more studies are needed to confirm this.
What is the difference between community exposure and community spread of the virus?Community exposure is being exposed to the risk by people who live around you in the community, rather than by someone who traveled from an area with infections. Community spread is when the virus is spreading among people in the general community in which you live.
I have seen posted on Facebook that gargling with a mixture of warm salt water or water/vinegar kills the coronavirus germs in the first four days when you start with the sore throat and am wondering if this is fact or fiction?Gargling salt water may improve sore throat symptoms, but it does not kill viruses and germs. If you are sick, you should stay home and limit your contact to others to avoid infecting them.
If someone dies and they are infected with COVID-19, can other people catch the virus from the body if there was an open casket viewing at the funeral?Per the CDC, there is currently no known risk associated with being in the same room at a funeral or visitation service with the body of someone who died of COVID-19. The CDC does currently recommend that people should not touch the body of someone who died of the novel coronavirus.
What treatment they are giving quarantined patients with this virus that are recovering (not on ventilators) so people at home under self-quarantine can do the same? Is it Tylenol, Advil, Vicks, Robitussin or just plain old chicken noodle soup and rest?There is currently no specific treatment for COVID-19. Several experimental drugs are undergoing clinical trials, which we can hopefully use in the near future. If a patient is infected with the virus and under quarantine, they can take medications to manage their symptoms, including acetaminophen, ibuprofen and any cough suppressant. There is currently no evidence to support that ibuprofen is worse than acetaminophen for patients with COVID-19. It is encouraged to drink fluids and rest as well. It is also important to take measures to avoid spreading the virus while a patient is under quarantine. The CDC website has good tips for doing this.
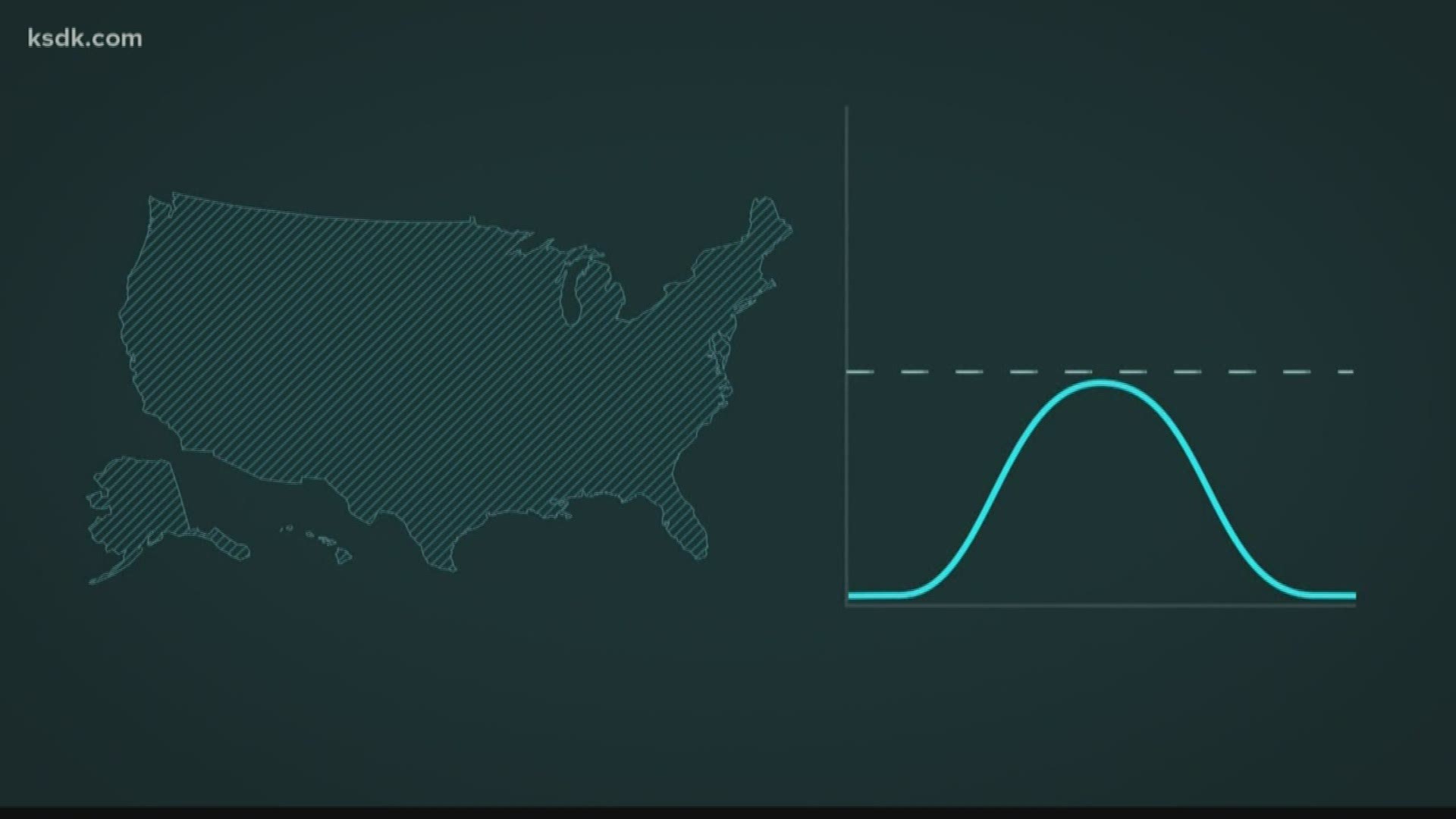
Flattening the curve is necessary to save lives, but will it extend the outbreak?"Flattening the curve" refers to delaying development of an outbreak by lowering infection rates. This is important so hospitals do not have a large surge of sick patients all at once and can better care for patients. This is done by implementing community mitigation strategies, like closing schools, which will reduce the number of overall cases and blunting the outbreak peak. The slow increase in cases over a longer period of time gives the healthcare system time to adapt.
I'm seeing posts that say the virus lives in the throat for 4 days and that gargling with salt water kills it.This is false. The incubation period (the time it takes for symptoms to develop) is thought to be between two and 14 days, but most commonly symptoms seem to emerge around five days. It is incorrect to suggest that people could cure themselves by gargling during this time. Although the virus is transmitted via respiratory secretions, there is no evidence that the virus remains in the throat and that gargling water (whether in plain form or as saline/vinegar) will help eliminate the virus. There also is no evidence that regularly rinsing the nose with saline can prevent respiratory infections, including COVID-19. There is a lot of misinformation concerning COVID-19, mostly coming from social media. Make sure you can fact check any information with verified sources such as CDC or WHO.
Is the coronavirus able to get into our water supply?The COVID-19 virus has not been detected in drinking water. Conventional water treatment methods that use filtration and disinfection, such as those in most municipal drinking water systems, should remove or inactivate the virus.
Because our skin serves as a protective organ, people with compromised skin due to conditions such as severe eczema or psoriasis can be at greater risk for infection. Does a compromised skin condition put one at any increased risk for contracting the coronavirus?The virus enters the body through the nose, eyes and inhaling through the mouth mainly through respiratory secretions from person-to-person. It does not infect the skin. Droplets from respiratory secretions can land on surfaces and remain viable for hours to days depending on different factors. The most important strategy to prevent getting sick is frequent hand washing as this will remove the virus from your skin and avoid it from reaching your eyes, nose, mouth. There is no evidence of increased risk due to compromised skin condition as long as you practice frequent hand washing.
Is the damage to the lungs because of the virus reversible after recovery or is it permanent?Most of the people that have been infected around the world have recovered. Some of them have had reduced lung function and experienced difficulty breathing with exercise. However, these patients can perform rehabilitation exercises to improve their lung capacity over time. It is still too early to establish long-term effects of the illness.
We've have heard so much info about what you should be doing about certain preventions, but my question is what should we be doing specifically in our everyday lives?Reasonable precautions that would be recommended in your everyday lives should include regular hand washing with soap and water and avoiding events with large crowds, especially events with large crowds indoors. If you have developed respiratory symptoms and are invited to a family gathering, it would be advisable to stay home. Although there hasn't been community transmission of the novel coronavirus proven within Missouri, all viruses that cause respiratory symptoms are spread through respiratory droplets in the same way as the novel coronavirus. If you are not sick, avoid contact with sick people. When out at a restaurant or shopping, avoid touching your eyes, nose, or mouth with unwashed hands and clean your hands often by washing them with soap and water for at least 20 seconds or using alcohol-based sanitizer that contains 60% alcohol.
If you have to use a public laundromat what precautions should you take, or should they be avoided completely?There are no specific precautions other than the above that need to be taken for laundromats and they do not need to be avoided. When washing clothes, the CDC recommends: "Read and follow directions on labels of laundry or clothing items and detergent. In general, using a normal laundry detergent according to washing machine instructions and dry thoroughly using the warmest temperatures recommended on the clothing label." Respiratory viruses such as coronavirus are spread through direct person-to-person contact. They are less commonly spread through indirect contact via contaminated surfaces. And when spread occurs indirectly, the risk is mainly with hard surfaces. The bottom line remains that good hand hygiene and avoidance of sick contacts are the key interventions, especially when out in public areas.
On average, how many weeks did it take for other countries to start seeing a decline in the number of cases?The first cases of coronavirus were reported in China at the end of December, 2019. The WHO declared the outbreak a Public Health Emergency of International Concern on Jan. 30, at which time the number of cases had increased to over 9000. With extremely aggressive public health measures including massive quarantine efforts, the construction of new hospitals, and widespread testing at no cost to the public, the number of new cases per day had decreased dramatically by mid-February. In contrast, Coronavirus was first detected in Italy in January, and until the third week of February there were only 3 reported cases. Today, Italy is reporting over 10,000 cases without any clear signs of slowing yet. The trajectory of the outbreak in the US is difficult to predict right now.
What criteria enabled the WHO to label this illness a pandemic?There was no specific threshold that was crossed that prompted the WHO to label this as a pandemic and there are no set cutoffs that differentiate an "epidemic" from a "pandemic." The decision was made based on a number of factors, most importantly the anticipated trend. Pandemic refers to the global outbreak of a new disease that is actively being transmitted in multiple different regions. Although this was as true of coronavirus last week as it is this week, the decision to officially label this event as a pandemic was based on global trends that show a sudden increase in the number of cases outside of China.
What are the recommendations for road trips, would this be discouraged along with all other non-essential travel?By avoiding airports and large crowds road trips would be expected to be lower risk than air travel. Non-essential travel to regions of the U.S. where there is known to be community spread of disease, including the Pacific Northwest, Northern California, Los Angeles and New York is definitely discouraged no matter the mode of transport.
If you think you might have coronavirus, whom do you call?If you are concerned about you or a family member having COVID-19, you should contact your family doctor and explain your symptoms. He or she may direct you to make an appointment or see another doctor for testing. This testing may be at a local clinic or at the local emergency department. If you feel sick, your goal should be to stay home and avoid getting others sick unless absolutely necessary. You should follow your doctor's instructions, contact your employer and do your best to avoid crowded areas while you are sick.
Any info on washing our bedding. Just hot water? Extra-long wash cycle? Extra rinse? Vinegar, bleach?The CDC has instructions for management of patients who have concern for, or confirmed, COVID-19:
We are hearing a lot about "social distancing," what exactly does that mean and how does it help prevent the spread of disease?Social distancing means remaining out of crowded places, avoiding large gatherings and maintaining distance (approximately 6 feet or 2 meters) from others when possible. As community transmission ramps up in a particular area, social distances measures will be increased as well. Are any special precautions required for food preparation to minimize the risk of coronavirus transmission? There is no evidence that COVID-19 can be transmitted to people through contact with food. These viruses should be killed by normal cooking temperatures. The most important preventative measure continues to be good hand hygiene with frequent hand washing. As always, people should follow normal food preparation practices including avoiding raw or under-cooked meats and unpasteurized dairy products. You should not share food, utensils or cups with a person known or suspected of having CVOID-19.
Is denatured alcohol, like what you get in a hardware store, an adequate disinfectant for surfaces?Denatured alcohol is commonly used as an industrial surface disinfectant and has anti-viral properties against some viruses including coronavirus. However, additional chemicals are added to these cleaners that can be toxic if absorbed through the skin. We would not recommend denatured alcohol for routine disinfectant use in the household. People should use household cleaners and EPA-registered disinfectants that are appropriate for the surface, following label instructions. Denatured alcohol should definitely not be used for hand washing. Alcohol solutions that are labeled as hand sanitizers are helpful if available but have not been shown to be any more effective than soap and water. To be effective, any hand sanitizer should contain at least 60 percent alcohol.
Does the pneumonia shot help prevent COVID-19 complications?The pneumonia shots, or Pneumovax and Prevnar vaccinations, are vaccines that help protect patients against a particular bacteria called Streptococcus pneumoniae (Pneumococcus), which commonly causes bacterial pneumonia in older patients or those with underlying lung or immune conditions. It does not provide any protection against viral infections.
If a pregnant woman has an appointment with her doctor at a hospital, should she be worried about an increased chance of being exposed to COVID-19?Hospitals and clinics are being proactive to screen patients for respiratory symptoms before they enter the facility to prevent any exposures. Pregnant women should practice the usual infection prevention techniques of hand washing and avoid those who are sick.
If the coronavirus is a respiratory illness, why are so many people buying toilet paper?There is concern that because toilet paper is manufactured in Japan there will be shortages. However, there is no evidence to suggest that supply will be interrupted. There is also fear that people will get quarantined in their homes, therefore, they feel the need to stockpile many different items including toilet paper. However, there is no current plan to quarantine people for prolonged periods of time.
If you are placed in isolation for two weeks with coronavirus, who clears you to go out in public again?The physician taking care of you as well as the state health department will let you know when it is okay for you to go out in public again.
Are newborns at higher risk? My daughter is about to have a baby and we're terrified that we should not allow visitors after the birth.At this time, there is no evidence to suggest that children are at higher risk. The usual infection prevention techniques should be used including frequently washing hands and avoiding people who are sick.
Is it true that black people can't get it because of the melanin in their skin?There is no evidence to support this claim. COVID-19 spreads person-to-person through respiratory droplets that land in mouths or noses or are inhaled into the lungs. Anyone who comes into close contact with someone infected is at risk of getting the infection.
How do people with compromised immune systems best protect themselves from COVID-19?For people with compromised immune systems the best way to protect yourself is to avoid people who are sick, avoid touching your eyes, nose and mouth, clean and disinfect frequently touched objects and surfaces using regular household cleaning products, wash your hands often with alcohol-based hand sanitizer or soap and water for at least 20 seconds.
What is the length of time from exposure to onset of symptoms and when can someone first test positive for the virus?Symptoms may appear between two and 14 days after exposure. We are still learning about the virus. Some studies of small groups of hospitalized people infected with the virus show that many have viral genes detected in their noses for at least seven days, and a few longer. We do not know if that means they are still infectious. The onset and duration of viral shedding and period of infectiousness for COVID-19 are not entirely known.
The virus is spread by droplets of spittle from infected people and passed around by coughing and sneezing. But some infected people are asymptomatic. Can people without symptoms spread the illness?People are thought to be most contagious when they are symptomatic. Asymptomatic infection has been reported and there might be some spread before people develop symptoms, but this is not thought to be the main way the virus spreads.
Can the coronavirus be spread by money?It is not certain how long the virus survives on surfaces or money. In general, coronaviruses do not survive well on surfaces and a recent study found that, of the surfaces studied, paper was the least likely surface to harbor virus.
What information do we know about the people who have died because of COVID-19? What percentage of them had underlying medical conditions?The data on mortality for COVID-19 is still a moving target and varies by age group and underlying health conditions. It appears that people with underlying lung disease, heart disease or other conditions that impair the immune system are more at risk. We do not have complete details about the medical conditions of every person who has died from COVID-19, but patients aged 65 years or older were more likely to have severe infections.
Is the coronavirus able to spread via recirculated air, like in office buildings, hospitals, public transit vehicles and our homes?According to researchers at Purdue University, COVID-19 could circulate inside cruise ship air conditioning systems. They say on aircraft, the coronavirus is more likely to spread by touch than through the air. And the World Health Organization says there is "very little risk" of any communicable disease being transmitted on board an aircraft.
The general public is being told not to wear face masks as they won't help keep us from getting sick, but health professionals are supposed to wear them. Why do the masks protect them but not us?Health professionals need to wear face masks because they are in very close contact with sick patients throughout the day as part of their job. It is also recommended that those who are taking care of someone who may have COVID-19 wear a face mask when in close contact. It is not recommended that people who are well wear a face mask as it is not the most effective way to protect yourself. The most effective way to protect yourself and others includes frequent hand washing with alcohol-based hand rub or soap and water, covering your cough with the bend of your elbow or tissue and maintaining distance from those who are coughing or sneezing.
Are infected people recovering?People also want to know what happens to people after they're infected with the virus. There's some good news here, according to Dr. Sean Whelan from Washington University's Department of Molecular Biology. "People are OK after they get the virus, 98% who get tested recover and then presumably are immune for the rest of their life," Whelan said.
Is it safe to travel?We've also received several questions about travel. You might need to change your plans, depending on where you're headed. Guidelines from the CDC are changing frequently. Click here for the latest information about travel within the U.S. and click here for the latest information about international travel and the outbreak.
Could my online orders carry coronavirus?People are worried about online orders from China, from sites like Amazon or Wish. But according to the Centers for Disease Control, there's little chance the virus would spread like this. There's no evidence that coronavirus in the US is associated with imported goods. So right now, don't worry about your online shopping habits.
Are there coronavirus tests available in St. Louis? If yes, will your regular physician have access to them in their office or does a patient have to go somewhere else for testing?
A healthcare provider will determine if a patient has signs, symptoms and the appropriate exposures compatible with COVID-19 and will then provide materials for testing. The decision on which patients receive testing should be based on the local epidemiology of COVID-19 as well as the clinical course of illness. |
| What Does Coronavirus Do to the Body? - The New York Times Posted: 26 Mar 2020 12:00 AM PDT  As cases of coronavirus infection proliferate around the world and governments take extraordinary measures to limit the spread, there is still a lot of confusion about what exactly the virus does to people's bodies. The symptoms — fever, cough, shortness of breath — can signal any number of illnesses, from flu to strep to the common cold. Here is what medical experts and researchers have learned so far about the progression of the infection caused by this new coronavirus — and what they still don't know. How does this coronavirus cause infection?The virus is spread through droplets transmitted into the air from coughing or sneezing, which people nearby can take in through their nose, mouth or eyes. The viral particles in these droplets travel quickly to the back of your nasal passages and to the mucous membranes in the back of your throat, attaching to a particular receptor in cells, beginning there. Coronavirus particles have spiked proteins sticking out from their surfaces, and these spikes hook onto cell membranes, allowing the virus's genetic material to enter the human cell. That genetic material proceeds to "hijack the metabolism of the cell and say, in effect, 'Don't do your usual job. Your job now is to help me multiply and make the virus,'" said Dr. William Schaffner, an infectious disease specialist at Vanderbilt University Medical Center in Nashville. How does that process cause respiratory problems?As copies of the virus multiply, they burst out and infect neighboring cells. The symptoms often start in the back of the throat with a sore throat and a dry cough. The virus then "crawls progressively down the bronchial tubes," Dr. Schaffner said. When the virus reaches the lungs, their mucous membranes become inflamed. That can damage the alveoli or lung sacs and they have to work harder to carry out their function of supplying oxygen to the blood that circulates throughout our body and removing carbon dioxide from the blood so that it can be exhaled. "If you get swelling there, it makes it that much more difficult for oxygen to swim across the mucous membrane," said Dr. Amy Compton-Phillips, the chief clinical officer for the Providence Health System, which included the hospital in Everett, Wash., that had the first reported case of coronavirus in the United States, in January. The swelling and the impaired flow of oxygen can cause those areas in the lungs to fill with fluid, pus and dead cells. Pneumonia, an infection in the lung, can occur. Some people have so much trouble breathing they need to be put on a ventilator. In the worst cases, known as Acute Respiratory Distress Syndrome, the lungs fill with so much fluid that no amount of breathing support can help, and the patient dies. What trajectory does the virus take in the lungs?Dr. Shu-Yuan Xiao, a professor of pathology at the University of Chicago School of Medicine has examined pathology reports on coronavirus patients in China. He said the virus appears to start in peripheral areas on both sides of the lung and can take a while to reach the upper respiratory tract, the trachea and other central airways. Dr. Xiao, who also serves as the director of the Center For Pathology and Molecular Diagnostics at Wuhan University, said that pattern helps explain why in Wuhan, where the outbreak began, many of the earliest cases were not identified immediately. The initial testing regimen in many Chinese hospitals did not always detect infection in the peripheral lungs, so some people with symptoms were sent home without treatment. "They'd either go to other hospitals to seek treatment or stay home and infect their family," he said. "That's one of the reasons there was such a wide spread." A recent study from a team led by researchers at the Icahn School of Medicine at Mount Sinai found that more than half of 121 patients in China had normal CT scans early in their disease. That study and work by Dr. Xiao show that as the disease progresses, CT scans show "ground glass opacities," a kind of hazy veil in parts of the lung that are evident in many types of viral respiratory infections. Those opaque areas can scatter and thicken in places as the illness worsens, creating what radiologists call a "crazy paving" pattern on the scan. Are the lungs the only part of the body affected?Not necessarily. Dr. Compton-Phillips said the infection can spread through the mucous membranes, from the nose down to the rectum. So while the virus appears to zero in on the lungs, it may also be able to infect cells in the gastrointestinal system, experts say. This may be why some patients have symptoms like diarrhea or indigestion. The virus can also get into the bloodstream, Dr. Schaffner said. Bone marrow and organs like the liver can become inflamed too, said Dr. George Diaz, section leader for infectious diseases at Providence Regional Medical Center in Everett, Wash., whose team treated the first U.S. coronavirus patient. There may also be some inflammation in small blood vessels, as happened with SARS, the viral outbreak in 2002 and 2003. "The virus will actually land on organs like the heart, the kidney, the liver, and may cause some direct damage to those organs," Dr. Schaffner said. As the body's immune system shifts into high gear to battle the infection, the resulting inflammation may cause those organs to malfunction, he said. As a result, some patients may endure damage that is inflicted not just by the virus, but by their own immune system as it rages to combat the infection. Why do some people get very ill but most don't?About 80 percent of people infected with the new coronavirus have relatively mild symptoms. But about 20 percent of people become more seriously ill and in about 2 percent of patients in China, which has had the most cases, the disease has been fatal. The disease can seriously sicken adults of all ages. According to a report of the first recorded cases in the United States, young, previously healthy adults can develop severe symptoms that could require ventilators and other life support. These patients may have a better chance at survival. Older, frailer people, or those with underlying health issues, like diabetes or another chronic illness, face the greater likelihood of dying from the virus. In China, Dr. Xiao conducted pathological examinations of two people who went into a hospital in Wuhan in January for a different reason — they needed surgery for early stage lung cancer — but whose records later showed that they had also had coronavirus infection, which the hospital did not recognize at the time. Neither patient's lung cancer was advanced enough to kill them, he said. One of those patients, an 84-year-old woman with diabetes, died from pneumonia caused by coronavirus, Dr. Xiao said the records showed. The other patient, a 73-year-old man, was somewhat healthier, with a history of hypertension that he had managed well for 20 years. Dr. Xiao said the man had successful surgery to remove a lung tumor, was discharged, and nine days later returned to the hospital because he had a fever and cough that was determined to be coronavirus. Dr. Xiao said that the man had almost certainly been infected during his first stay in the hospital, since other patients in his post-surgical recovery room were later found to have coronavirus. Like many other cases, it took the man days to show respiratory symptoms. The man recovered after 20 days in the hospital's infectious disease unit. Experts say that when patients like that recover, it is often because the supportive care — fluids, breathing support, and other treatment — allows them to outlast the worst effects of the inflammation caused by the virus. What do scientists still not know about coronavirus patients?A lot. Although the illness resembles SARS in many respects and has elements in common with influenza and pneumonia, the course a patient's coronavirus will take is not yet fully understood. Some patients can remain stable for over a week and then suddenly develop pneumonia, Dr. Diaz said. Some patients seem to recover but then develop symptoms again. Dr. Xiao said that some patients in China recovered but got sick again, apparently because they had damaged and vulnerable lung tissue that was subsequently attacked by bacteria in their body. Some of those patients ended up dying from a bacterial infection, not the virus. But that didn't appear to cause the majority of deaths, he said. Other cases have been tragic mysteries. Dr. Xiao said he personally knew a man and woman who got infected, but seemed to be improving. Then the man deteriorated and was hospitalized. "He was in I.C.U., getting oxygen, and he texted his wife that he was getting better, he had good appetite and so on," Dr. Xiao said. "But then in the late afternoon, she stopped receiving texts from him. She didn't know what was going on. And by 10 p.m., she got a notice from the hospital that he had passed." |
| You are subscribed to email updates from "asthma attack symptoms child,mucus in stool" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |
Comments
Post a Comment