Community Spotlight: Excuse my dry cough - The Edwardsville Intelligencer
Community Spotlight: Excuse my dry cough - The Edwardsville Intelligencer |
- Community Spotlight: Excuse my dry cough - The Edwardsville Intelligencer
- Photos: COVID-19 Survivors Journal Symptoms and After Effects - NBC 7 San Diego
- Asthma Latest Facts: Causes, Symptoms, Prevention and Treatments - Gilmore Health News
| Community Spotlight: Excuse my dry cough - The Edwardsville Intelligencer Posted: 24 Jul 2020 07:12 PM PDT  Coughing is one of the body's natural defense mechanisms. It is a reflexive action that helps to facilitate the clearance of particulate matter, accumulated secretions, and irritants from the respiratory tract. A cough can serve as a warning for both respiratory and non-respiratory diseases and is one of the most common reasons for individuals to seek medical care. One important type of cough is known as a dry or nonproductive cough. This type of cough does not produce phlegm or mucus https://www.healthline.com/health/dry-cough. In contrast, a productive or wet cough https://www.healthline.com/health/wet-coughproduces phlegm or mucus and is often due to bacterial or viral infections. With a wet cough, physicians can test a sample of the patient's sputum, or phlegm, in order to reach a diagnosis. The cause of a dry cough, however, may more difficult to determine. Having a dry cough on occasion is often normal; however, one that is persistent may be a sign of a more serious underlying condition. In the time of COVID-19 a dry cough is one of the leading symptoms of cases. It's important for you to consider the below factors in regards to seeking medical attention: Cough duration Physicians classify a cough based on several factors. One such factor is the duration. The symptoms of a cough often get worse, depending on how long the cough persists. In this way, coughs are classified as acute, subacute, or chronic. An acute cough lasts less than three weeks, while a subacute cough may last anywhere between three to eight weeks. Both are in contrast to a chronic cough, which lasts longer than eight weeks https://www.rightdiagnosis.com/sym/nonproductive_cough.htm.7 As stated previously, a chronic dry cough may indicate a more severe condition. Common causes of dry cough Several medical conditions are associated with a chronic dry cough, and in accordance, a dry cough may present with many other symptoms https://pubmed.ncbi.nlm.nih.gov/29080708/. For example, a dry cough with wheezing, shortness of breath, and a whistling sound upon exhalation may point to asthma https://www.nhlbi.nih.gov/health-topics/asthma, which is an inflammatory disease of the respiratory tract. A variant of asthma, called cough-variant asthma (CVA), however, is not associated with typical asthma symptoms. In CVA, patients only present with a chronic dry cough and increased airway inflammation. Chronic dry cough may also be found in gastroesophageal reflux disease (GERD), which presents with difficulty swallowing, a burning sensation in the chest or upper abdomen, and bad breath. As many as 40% of GERD patients report having a chronic dry cough. However, up to 75% of people with a chronic dry cough related to GERD, may not have the typical gastrointestinal symptoms of GERD. Therefore, based on a cough alone, GERD may be a complicated syndrome to diagnose. Other causes of chronic dry cough are postnasal drip and viral infections. With postnasal drip, patients usually have a chronic cough, along with runny nose, sore throat, and frequent swallowing. This syndrome is caused by mucus build up in the back of the nose and throat and is commonly associated with a viral infection, asthma, or even GERD https://www.healthdirect.gov.au/post-nasal-drip. Viral infections causing an upper respiratory infection can be associated with a dry cough that may linger long after other symptoms, such as runny nose, sore throat, muscle aches, and fever, have improved. These types of coughs can go away with time. Less common causes of dry cough can include idiopathic pulmonary fibrosis, lung cancer https://www.mesolawsuitafterdeath.com/mesothelioma/does-mesothelioma-asbestos-cancer-cause-a-cough/, cigarette smoking, exposures to irritants, such as chemicals, pollution, or dust, allergies, and even medications (eg, ACE inhibitors). In some cases, a dry cough may even go unexplained. In order to come to a proper diagnosis, it is essential to take into consideration a whole medical history and associated symptoms. Temporary dry coughs are most likely benign, however, coughs that linger for weeks to months, get worse, or start to produce blood or mucus may require a more thorough examination. Vamsi Ahobila, MD obtained a medical degree from Ross University School of Medicine in 2016. Since that time, Vamsi has helped co-author publications and clinical textbooks in the fields of Obstetrics and Gynecology and Critical Care Medicine. He owns and operates ProScriptMD. |
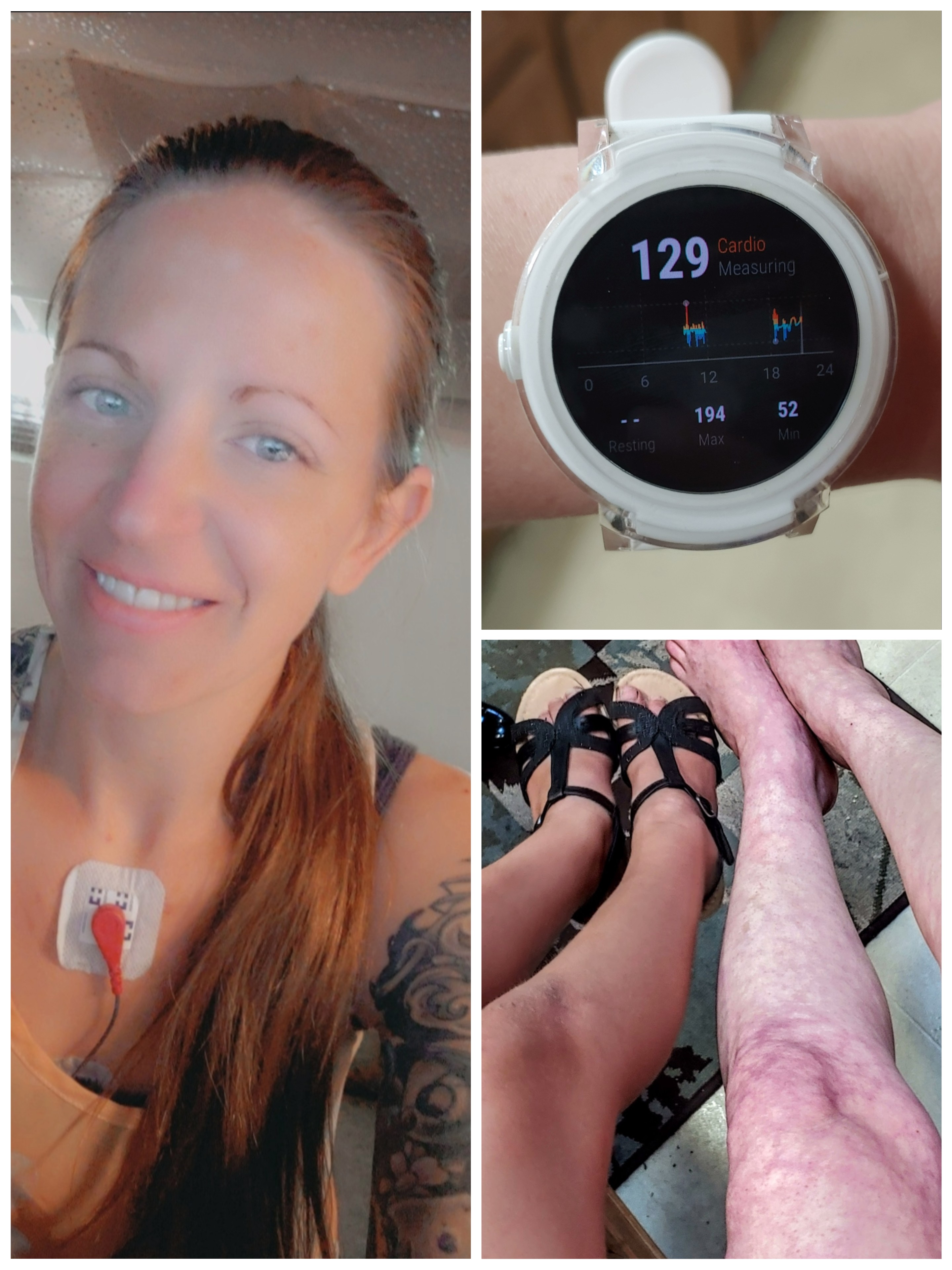
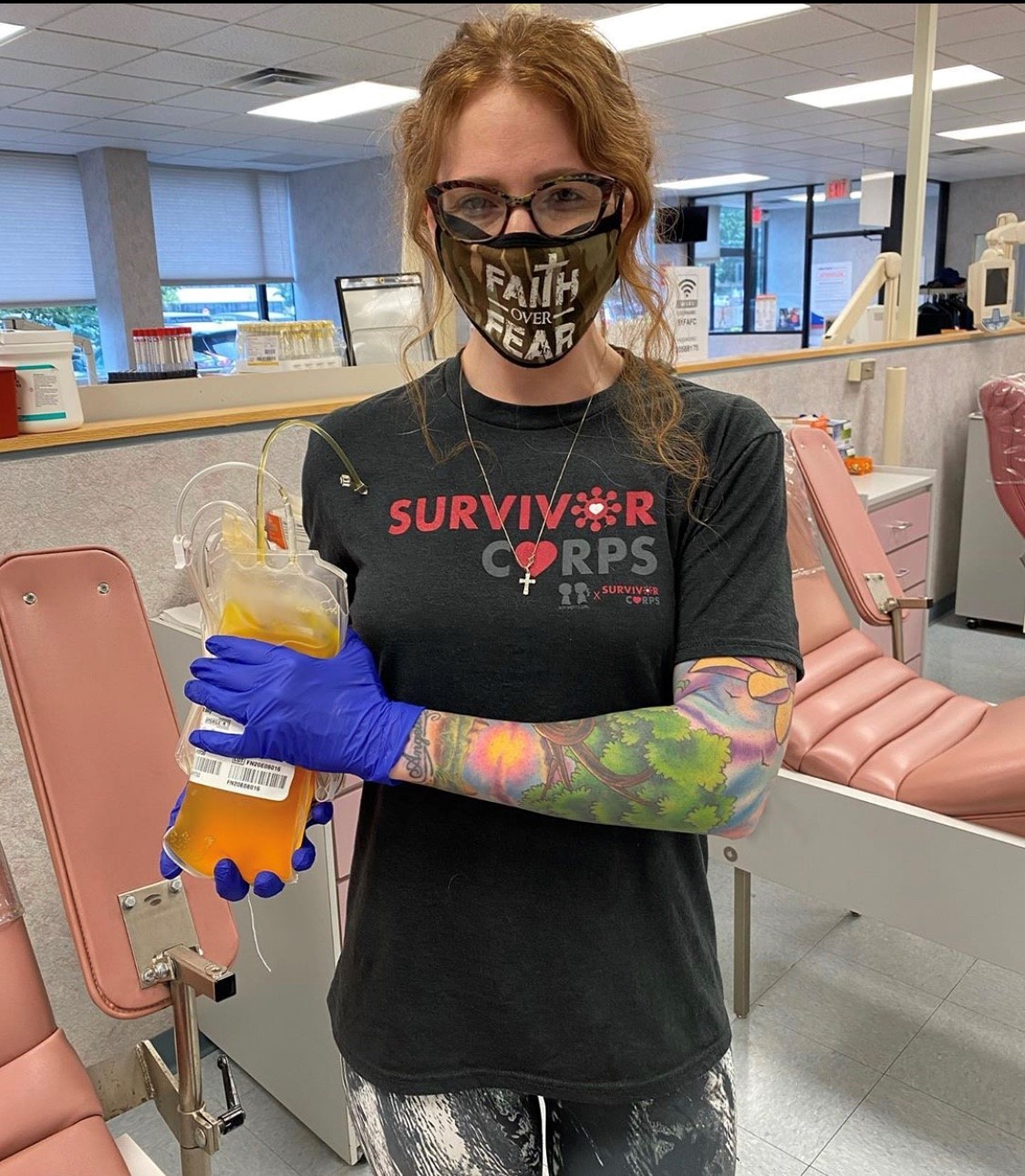
| Photos: COVID-19 Survivors Journal Symptoms and After Effects - NBC 7 San Diego Posted: 30 Jul 2020 07:26 PM PDT A collection of stories from people across the country explaining in their own words living with the long-term complications of COVID-19. They are part of an 80,000+ member support group on Facebook called Survivor Corps |
| Asthma Latest Facts: Causes, Symptoms, Prevention and Treatments - Gilmore Health News Posted: 27 Jul 2020 06:53 AM PDT Table of Contents Asthma is a disease characterized by a more or less pronounced inflammation of the airways, bronchi, and bronchioles. It leads to breathing difficulties, shortness of breath, wheezing, and a feeling of tightness in the chest. Asthma Inhaler Asthma is a chronic disease that manifests most often through sudden attacks separated by periods of normal breathing. However, in some people, asthma leads to persistent breathing difficulties that interfere with daily activities. Asthma is often associated with an abnormal reaction of the airways to various stimuli (allergens in the air, smoke, perfumes, etc.). Asthma attacksAn asthma attack is a sudden worsening of symptoms. In many people, asthma manifests itself in occasional attacks with normal breathing between the attacks. An asthma attack often begins with a dry cough, followed by breathing difficulties that cause a clearly audible wheeze. It is usually accompanied by sputum. During an attack, the opening of the bronchi is narrowed by a strong inflammatory reaction and contraction of the muscles in the lining of the bronchi. Attacks can be effectively relieved with medication. However, they are potentially dangerous, especially in fragile people (elderly people suffering from respiratory infections, etc.). Read Also: Transplantation: Damaged Lungs Restored With Live Pig's Blood PrevalenceSince the 1960s, asthma has steadily increased in industrialized countries. It is estimated that 1 in 13 Americans have asthma or about 25 million people. Two stages in life seem to be more prone to the onset of asthma: childhood and the early forties. One in eight children with asthma (8-12% of children aged 11 and under) has asthma symptoms. This is usually one of the first chronic diseases of childhood. Fortunately, about half of these children will become completely asymptomatic during adolescence. They will still be at risk though. CausesThe causes of asthma are not well known, although it is known that there are both genetic and environmental risk factors. Inflammation of the airways leads to the production of thick mucus in the bronchi, which obstructs the flow of air. At the same time, the muscles around the bronchi contract, causing the bronchi to "narrow" (bronchospasm). This causes breathing difficulties. Asthma is associated with respiratory allergies in about 80% of cases but is not always of allergic origin. People with asthma have an excessive sensitivity of the bronchi (hyper-reactivity) to one or more substances. The following factors can help trigger an asthma attack or aggravate breathing difficulties, but they are not the cause of asthma:
Read Also: Study Reveals The Crucial Role Of Immunotherapy In Lung Fibrosis Degree of severityFor some people, asthma attacks are rare and do not have a serious impact on everyday life. However, asthma can become more severe if the attacks are frequent and the symptoms are intense. In some cases, breathing difficulties and shortness of breath may persist between attacks. Here are some signs of severe or poorly controlled asthma:
Possible complicationsPoorly controlled asthma can cause permanent symptoms. In exceptional cases, it can become complicated with shortness of breath and endanger the lives of those affected. Every year in the US about 3,564 people die from asthma attacks. Most of these deaths could be prevented by good management of the disease. The vast majority of people with asthma can, therefore, live normally, as long as they follow their treatment correctly. On the other hand, attacks rarely occur suddenly and without warning. If you learn to recognize these signs, you can take timely action to reduce the severity of attacks. Read Also: Novel Nanoparticles Approach To Lung Tumors May Eradicate The Side Effects Of Chemo Asthma symptomsThe symptoms may be intermittent or persistent. They can occur after training or when another triggering factor is present and are usually more pronounced at night and early morning.
Note. For some people, asthma is simply a persistent cough that often occurs at bedtime or after physical exertion. Alarm signals in case of an attack During an asthma attack, the symptoms of shortness of breath, coughing, and secretions of mucus get worse. If the following symptoms are also present, it is imperative to ask for help or go to the emergency room to control the attack as soon as possible:
Read Also: COVID-19: Double Lung Transplantation Saves Young Patient in the US People and risk factors for asthma
Risk FactorsThe increase in the number of asthmatics in recent decades may be due to the following external factors:
Read Also: Tobacco: the Lungs May Partially Self-Repair After Smoking Cessation Preventing asthmaThe treatments aim to make the symptoms of asthma disappear, but in some people, asthma is still a chronic disease with phases of improvement and worsening. Sometimes asthma disappears after adolescence, especially if it was properly treated in childhood and there is no allergic cause. At present, the only basic preventive measure recognized is to avoid active and passive smoking. Tobacco smoke irritates the airways and is a breeding ground for respiratory diseases. There is currently no known measure to prevent asthma; there is no medical consensus on this issue. Consuming the right amount of fruit and vegetable fiber can help prevent asthma. The development of asthma depends on the amount of fruit and vegetables consumed. Intestinal bacteria ferment fibers in the digestive tract of fruit and vegetables. This helps to transport the fatty acids in the blood, which influence the immune response in the lungs. Breastfeeding a child also provides some protection against asthma. This seems to be related to allergenic products that, when consumed by the mother during breastfeeding pass into the milk and lead to tolerance to these allergenic substances. Measures for early detectionAsthma can be detected early on by spirometry testing. These are measurements of lung capacity (e.g., the volumes and rates of airflow passing through the lungs as you breathe in and out), which are measured with a spirometer. The patient simply blows into a small electronic device with a nozzle. Spirometry has been used for many years in the diagnosis of asthma and chronic obstructive pulmonary disease (COPD). This examination is performed on a doctor's prescription, in a pulmonologist's office or in a hospital. Read Also: Vaping: Devastating Effects on the Lungs Measures to reduce the intensity and frequency of attacksDesensitization treatmentIf asthma is closely related to allergies, desensitization treatment can help prevent asthma attacks. This requires allergy testing to detect the substance causing the symptoms. General MeasuresDevelopment of an action plan. Find out from your doctor the factors that cause attacks and avoid them as much as possible: allergies, activities, behavior, etc. Pay attention to the warning signs of worsening asthma so that you can act quickly as per your doctor's advice. These signs may vary from one person to another:
It is important that an asthmatic always take his medication with him so that he can relieve the symptoms at the beginning of the seizure and prevent them from getting worse. Children with asthma should also have their inhaler handy at school. If your child has asthma, it is a good idea to inform teachers so that they can help the child in case of an attack. Read Also: Lung Cancer: Nicotine May Promote the Development of Brain Metastases Check for mold, pets, pollen, and other respiratory irritants, especially if the asthma is from an allergic source. The mold is usually found in damp and excessively isolated rooms; to combat it, the rooms should be well ventilated; If you are allergic to pets, the best solution is to remove the pets from the house; Avoid exposure to pollen by keeping the windows of the house closed. Make sure the filters of the indoor ventilation units are clean to ensure proper recirculation of indoor air; Avoid exposure to respiratory irritants. Control dust mites. Dust mites feed mainly on dead skin fragments and grow in hot and humid environments. In case of allergy:
Read Also: Mesothelioma: A Promising New Treatment Extends Life Expectancy People with well-controlled asthma should not stop exercising – quite the opposite! Regular moderate outdoor exercise and breathing exercises are recommended. Regular exercise improves lung capacity and bronchial dilation and gradually reduces the threshold for stress-induced asthma. In addition, physical activity at any age improves the quality of life and reduces stress. However, individual and endurance sports cause more asthma attacks than team sports. Asthma can be partially prevented by warming up before sustained effort and gradually reducing the effort at the end of the exercise period. People who react to cold, dry air can cover their mouth and nose with a tissue that warms and humidifies the air they breathe. If these preventive measures are not sufficient, an inhaled bronchodilator should be used 10 to 15 minutes before exercise. If asthma induced by exercise is too severe, this may mean that the overall treatment is not appropriate. You should discuss this with your doctor. Take some time to relax. Sometimes stress or anxiety can cause asthma attacks. In this sense, anything that helps to reduce stress and anxiety, such as deep breathing, massage, etc., helps to control the disease better. Asthma treatmentAsthma is often a chronic disease that requires regular treatment even between attacks. The medicines used to control asthma do not provide a permanent cure. They facilitate breathing by increasing the opening of the bronchi (bronchodilation) and reducing inflammation. Most of them are taken by inhalation, which allows them to act quickly and with as few side effects as possible. The doctor also tries to administer the smallest dose of medicine to control the symptoms with the best tolerance of the treatment. Read Also: Aspirin Protects the Lungs Against Pollution According to Study However, despite the effectiveness of the treatments, 6 out of 10 asthmatics cannot control their symptoms. The main causes are poor understanding of the disease, fear of side effects, and forgetting to take the medicine. However, the side effects of inhalation treatments are minimal compared to the risks associated with severe and frequent asthma attacks. The use of inhalation devices seems simple but requires a specific technique to be effective. However, less than half of asthmatics use their inhalers correctly. The different inhalers (metered-dose inhalers, dry powder inhalers, and nebulizers) each have their own mode of use. Your doctor and pharmacist can explain the correct way of use to you. Metered-dose inhalers: Shake the aerosol well and keep it upright. After gently emptying the lungs, inhale slowly and deeply through the mouth and release the aerosol in the first second of inhalation. Then hold your breath for 5 to 10 seconds and exhale slowly. Dry powder inhalers: These systems are easier to use because they do not require coordination of inspiration and triggering. You should inhale as firmly and quickly as possible, hold your breath for 10 seconds and then exhale outside the inhaler. Inhalation chambers: These are used with inhalers for children under 8 years of age and the elderly. For babies, inhalation is done with a face mask, which should be kept on the face for at least 6 calm breaths. Asthmatics are increasingly involved in monitoring their respiratory status. For example, people suffering from severe asthma can measure their maximum expiratory flow at home to adjust their own treatment according to the results. The training must have been completed in advance. Read Also: Recent Study Shows That Lung Cancer Is Under-Recognized in Non Smokers Asthma DrugsThere are 2 categories of medicines used to control asthma symptoms. The first types are rescue medicines that must be taken when symptoms occur. They provide immediate relief but do not relieve bronchial tube inflammation. The other medications are taken to control the diseases long term. They should be taken daily, even if there is no difficulty breathing. They reduce bronchial tube inflammation and decrease the frequency of attacks. If they are not taken regularly, the frequency and severity of attacks will increase, as will the need for rescue medications. Many people with asthma do not fully understand the difference between treating attacks and controlling them. Make sure you understand what each of your medicines is for and how often you need to take them. Treating an attackAttack drugs are referred to by a variety of terms, including fast-acting bronchodilators or short-acting beta2 agonists. They are only used to relieve symptoms of attacks(coughing, tightness in the chest, wheezing, and shortness of breath) or before stress-induced physical exertion on asthma. For mild and intermittent asthma, the treatment of attacks may be the only medicine needed. These medicines include salbutamol ((Ventoline®, Ventilastin®, Airomir®, Apo-Salvent®, New Salmol®) or terbutaline (Bricanyl®). They are taken by inhalation and widen the airways very quickly, namely in 1 to 3 minutes. There are few side effects with occasional use, but high doses can cause tremors, nervousness, and an increase in heart rate. If you feel the need to take them frequently (usually more than three times a week), this means that your asthma is not being controlled properly. In this case, it will be necessary to use disease-modifying medication to treat the inflammation. It is important that a person with asthma always carries his or her bronchodilator with them because an asthma attack can happen anywhere. Take it as soon as the first symptoms of an attack appear and wait at least 30 seconds between inhalations. Inhaled ipratropium bromide (rare). It is an anticholinergic that blocks the action of a chemical that causes the muscles of the airways to contract. It is less effective than inhaled beta2 agonists and is sometimes used for intolerance to inhaled beta2 agonists. It takes 1 to 2 hours to achieve maximum effect. Drugs for controlUnlike rescue medications, control medications do not immediately relieve symptoms. They work slowly and are effective in the long term to reduce inflammation and the frequency of seizures. It is therefore important to take them daily. Corticosteroids: Corticosteroids reduce inflammation in the airways and therefore decrease mucus production. They are usually taken daily in small doses by inhalation (e.g. Alvesco® and Pulmicort®). The doctor prescribes the lowest possible effective dose. They can also be taken in tablets for severe asthma for a short period of several days (e.g. prednisolone, methylprednisolone). Regardless of whether they are taken by inhalation or in the form of tablets, they work in the same way, but inhalation allows much lower doses, a much more localized effect, and therefore fewer side effects. This class of medication is the most effective in controlling asthma. Its effect is felt after a few days of use. Read Also: Genomic Analysis May Detect Lung Cancer Before It Even Develops Side effects Corticosteroids inhaled at moderate doses have few side effects, even when taken over a long period of time. The most common side effects are hoarseness of voice or the appearance of thrush (or candidiasis, caused by yeast that forms white patches on the tongue). For this reason, rinse your mouth after each dose. Corticosteroid tablets have serious long-term side effects (weakening of the bones, increased risk of cataracts, etc.). They are reserved for cases of severe asthma in combination with other treatments. Long-acting bronchodilators: These are prescribed in combination when inhaled corticosteroids alone are not sufficient to control the symptoms of asthma. Long-acting beta2 agonists cause bronchodilation for 12 hours. Their efficacy can be rapid in 3-5 minutes as Formoterol® (e.g. Foradil®, Asmelor®) or slower after 15 minutes as Salmeterol (Serevent®). They are used in combination with a corticosteroid. There are inhalers that combine both types of drugs, such as Seretide® (Fluticasone propionate / Salmeterol). Combinations with formoterol (Symbicort®, Innovair®, and Flutiform®) can also be used as a rescue drug, although they are also effective for long-term inflammation. Antileukotrienes: Taken orally, they reduce the inflammation caused by leukotrienes, substances that contribute to the inflammatory response. They can be used alone or in combination with inhaled corticosteroids. They are indicated for the prevention of exercise-induced asthma, mild asthma, for people whose asthma is not controlled by inhaled corticosteroids alone, and for people who abuse their sprays. Theophylline: This is the oldest bronchodilator (e.g. Theostat®). It is rarely used today because effective dosage without side effects is hard to find. It can be prescribed as a pill for people who have difficulty taking the sprays. Anti-Immunoglobulin E: This class of medicine is intended to treat severe allergic asthma in people whose asthma is difficult to control with other treatments. Omalizumab (Xolair®) is administered by subcutaneous injection once or twice a month. It is really important to use a controlled medicine according to your doctor's instructions, even if you have no symptoms. Without regular use, bronchial inflammation will continue and asthma attacks are likely to become more frequent. If a person has asthma, they shouldn't accept symptoms without doing something. For example, not tolerating shortness of breath, slight coughing, or difficulty breathing at night. The disease should not progress because if you get tired of it, you can avoid treatment and over time it can degrade the bronchial tubes, which can lead to a permanent worsening of symptoms and, in serious cases, frequent superinfections and hospital stays. It is best to work with your doctor to find an effective treatment. Read Also: COVID-19 Breakthrough: An Inhaled Drug May Reduce the Risk of Complications by 79% This is especially important for parents of children with asthma. They are often reluctant to give their children medication, and this is understandable. But in this case, they are wrong. These children must have the opportunity to develop their respiratory capital properly so that they can use it as adults. Even a child who shows signs of untreated asthma sleeps poorly has difficulty playing a sport and grows poorly. The treatment makes them feel better and saves their bronchial tubes for the future. Complementary approaches to asthma treatmentA comprehensive preventive approach, including lifestyle changes, allows some people to reduce their medication use. The unconventional approaches presented here aim to improve the quality of life of people with asthma by reducing the frequency of attacks. They do not relieve an acute attack and should be used in addition to controlling drugs if they are still needed. Yoga: Yoga can help to reduce the consumption of medication by asthmatics of all ages, improving their quality of life both psychologically (good mood, positive attitude, self-confidence, etc.) and physiologically (muscle relaxation, mobility, and joint strength, the health of coronary arteries, etc.). Yoga can also help to reduce the risk of asthma attacks. As yoga safety is well established, it seems to be an interesting and cost-effective therapeutic intervention that can be used to complement conventional asthma therapy. Possible effectiveness of the Buteyko method: The Buteyko method is a breathing technique developed in Russia in the 1950s by Dr. Buteyko. According to Dr. Buteyko's view, asthmatics are in chronic hyperventilation; their CO2 levels in blood and alveoli are too low. The breathing exercises developed by Dr. Buteyko should help people breathe better and a little slower. According to practitioners of this method, these exercises have helped many asthmatics to improve their quality of life after a few days. A systematic review to evaluate the effectiveness of the Buteyko method on asthmatics was published in 2005. In general, breathing exercises seem to improve the quality of life and reduce asthma symptoms, as a 2009 clinical study showed. However, the positive effects were only noticeable after 6 months. Read Also: Study Shows That an L. Casei Spray Could Be Helpful in the Treatment Chronic Sinusitis Possible efficacy Vitamins A, C, and E: Numerous studies have shown an association between asthma and low blood levels of antioxidant vitamins (vitamin A, vitamin C, and vitamin E). Several studies have investigated the efficacy of oral intake of such supplements in relieving asthma symptoms in people exposed to high levels of air pollution. The largest study involved 158 asthmatic children living in Mexico City. For one year, one group took vitamin C supplements and another group took a placebo. Some parameters of lung function, which were evaluated weekly, improved with the intake of vitamins C (250 mg per day) and E (50 mg per day). However, this efficacy is controversial as others have not demonstrated any benefit from this supplement. Further clinical trials are therefore required. Note: Cigarette smoke reduces levels of vitamins C and E in the lungs. Vitamin C supplements may reduce exercise-induced asthma but there is little scientific evidence to support this recommendation. In one study, participants received 500 mg of vitamin C (or placebo) two days before the training. Taking vitamin C reduces bronchial contraction during exercise. However, in 2009, a meta-analysis concluded that there were not enough reliable clinical trials to recommend such a supplement. Acupuncture: A systematic review and a meta-analysis published in 2004 concluded that there was not enough evidence to recommend acupuncture for the treatment of asthma. Although some studies suggest that acupuncture can be effective, the results are contradictory and the quality of the studies is often insufficient. Flavonoid-rich foods. Flavonoids, including luteolin, apigenin, or quercetin, have anti-allergy (achieved by inhibiting the release of histamine), anti-inflammatory, and antioxidant properties. Several studies have shown that asthma is less frequent in people with high dietary intake of flavonoids, particularly those who consume high fruit and vegetable diets. Chiropractic: According to 3 systematic reviews, there is no evidence that chiropractic can be an effective treatment for asthma although some people have benefited from it. Homeopathy: There is little published scientific research on the effects of homeopathy on asthma. A team at the University of Glasgow, Scotland, showed that a dose of 30 CH of pollen and dust mites was more effective than a placebo in treating hay fever and asthma respectively. In addition, a meta-analysis demonstrating a positive effect is controversial, and a study of 186 people suffering from asthma caused by dust mite allergies concluded that the homeopathic treatment given was ineffective. In 2004, a meta-analysis, in which 6 studies and 556 patients were regrouped, concluded that the data were insufficient to conclude that homeopathy was effective against asthma. Read Also: Cancer Latest Facts: Types, Causes, Symptoms, Prevention, Risk Factors and Treatments Fish oils: Researchers believe that the low level of omega-3 fatty acids in the diet of the western population, due in particular to omega-6 fatty acids, could be a cause of the increased number of cases of allergic diseases in modern societies (asthma, allergic rhinitis, skin allergies, atopic eczema, etc.). Currently, this is only a hypothesis. About twenty small-scale studies on asthma have been carried out: The results are mixed and the data set does not allow any conclusions to be drawn on the effectiveness of fish oils. Although several studies produced encouraging results a meta-analysis of 10 randomized trials conducted in 2006 showed that it was impossible to conclude that omega-3 supplements are effective in asthma. Autogenic training: A meta-analysis of 60 studies (including 35 randomized controlled trials) defined the diseases for which autogenic training is particularly effective. Asthma is one of them. However, these results are based on only a few asthma studies: 3 randomized controlled trials involving a total of 93 subjects. The beneficial effects reported include improved pulmonary function, reduced anxiety, and reduced need for medication. Pycnogenol: Several preliminary studies conducted on a small number of people with asthma suggest that Pycnogenol may be useful in treating this condition. For example, a study of 60 young people aged 6 to 18 years with mild to moderate asthma showed that taking Pycnogenol (1 mg/lb body weight) for 3 months reduced the symptoms of asthma and the use of bronchodilators. Ivy leaf extract (Hedera Helix): Ivy is believed to promote mucus excretion and reduce bronchial spasms. A systematic review conducted in 2003, including 3 clinical trials, showed that ivy extracts-based preparations improved respiratory function in asthmatic children. Chinese medicine: Numerous studies and meta-analyses have examined the efficacy of Chinese herbal preparations for the treatment of asthma. Several appear to have beneficial effects, including Mai-Men-Dong-Tang and Liu-Wei-Di-Huang-Wan. Boswellia (Boswellia serrata): Boswellia resin, which comes from the trunk of this large tree native to India, is used in Ayurvedic medicine to treat inflammation of the respiratory tract. It appears that the Boswellia resin inhibits the production of certain pro-inflammatory substances in the human body, especially leukotrienes, which intervene specifically in bronchoconstriction. A preliminary study suggests that Boswellia improves respiratory function in asthmatics. Read Also: Virus Pandemic Health Implications for Mesothelioma Patients Gingko Biloba: A preliminary study showed that Gingko Biloba leaf concentrate improves pulmonary function in asthmatics. Several studies in rats support the efficacy of Gingko in reducing bronchial tube inflammation. Lobelia (Lobelia Inflata): Lobelia flowers have traditionally been used internally to treat certain respiratory diseases such as asthma and chronic bronchitis. They facilitate breathing by promoting mucus excretion and reducing bronchial spasms. A meta-analysis published in 2010 reports the positive effects of this plant on the symptoms and respiratory function of asthmatics. Its use is limited in time by gastrointestinal side effects. Warning: In high doses, the plant can cause vomiting and is poisonous. Dietary recommendationsEliminate allergens from food. Food allergies are thought to cause or aggravate bronchial obstruction in 2% to 8.5% of children with asthma. A reaction to food is thought to trigger an immediate or "delayed" asthma attack. Eggs, fish, shellfish and crustaceans, nuts and peanuts could trigger an immediate attack, while cow's milk, chocolate, wheat, citrus fruits, food additives (dyes, preservatives, sulfites, etc.), soybeans, lemons, and corn could do so with a delay. The introduction of a rotating diet can help identify allergenic foods that can trigger asthma. Read Also: COVID-19: A Nasal Spray Made From Seaweed Extracts Could Prevent Infection Note: Several clinical studies have examined tartrazine (yellow #5, one of the most commonly used food colors), which is suspected of triggering allergies. In 2001, a synthesis of 6 randomized controlled trials concluded that most asthmatics who exclude tartrazine from their diet see no benefit. People who are particularly sensitive to tartrazine are rare. Avoid pro-inflammatory foods: saturated fats (mainly in animal products: meat, poultry, and dairy products), refined products, and sugars as they contribute to bronchial obstruction. Choose fresh vegetables, whole grains, legumes, onions, and garlic (unless you are allergic to them). Onions and garlic are rich in vitamin C and quercetin, two substances said to have an anti-allergy effect. Magnesium: In conventional medicine, magnesium is administered intravenously in the event of an acute attack, but the results of 2 clinical studies involving more than 300 subjects suggest that magnesium has no clinical effect on asthma symptoms. Referenceshttps://www.aaaai.org/conditions-and-treatments/asthma Pycnogenol((R)) in the Management of Asthma Herbal medicines for asthma: a systematic review Children's lung function and antioxidant vitamin, fruit, juice, and vegetable intake The attenuation of exercise-induced bronchospasm by ascorbic acid N-3 polyunsaturated fatty acids and allergic disease Sahaja yoga in the management of moderate to severe asthma: a randomised controlled trial Effect of two breathing exercises (Buteyko and pranayama) in asthma: a randomised controlled trial Acupuncture for chronic asthma Chiropractic care in asthma and allergy Treating asthma with omega-3 fatty acids: where is the evidence? A systematic review Is evidence for homoeopathy reproducible? Autogenic training: a meta-analysis of clinical outcome studies |
| You are subscribed to email updates from "homeopathic remedies for asthma,phlegm" - Google News. To stop receiving these emails, you may unsubscribe now. | Email delivery powered by Google |
| Google, 1600 Amphitheatre Parkway, Mountain View, CA 94043, United States | |


























Comments
Post a Comment