Strep throat: What to know about Group A Strep this winter - USA TODAY
Experts explains how Strep A can affect children, adults
Several children in the United Kingdom have died after being infected with Strep A. Here's what you need to know about the virus.
Anthony Jackson, USA TODAY
It's been an unprecedented start of the winter for those of us working on the front lines, particularly in pediatric emergency rooms and children's hospitals. After COVID-19 mitigation methods suppressed the usual seasonal surges from 2020 to 2021, the past few months have been marked by an uptick in RSV, flu and other respiratory viral illnesses in children.
But there is good news. Nationally the rate of RSV has been declining since November. And influenza, which burst onto the scene two months earlier than usual, is now on the decline in many parts of the country; perhaps signaling an early peak to the flu season.
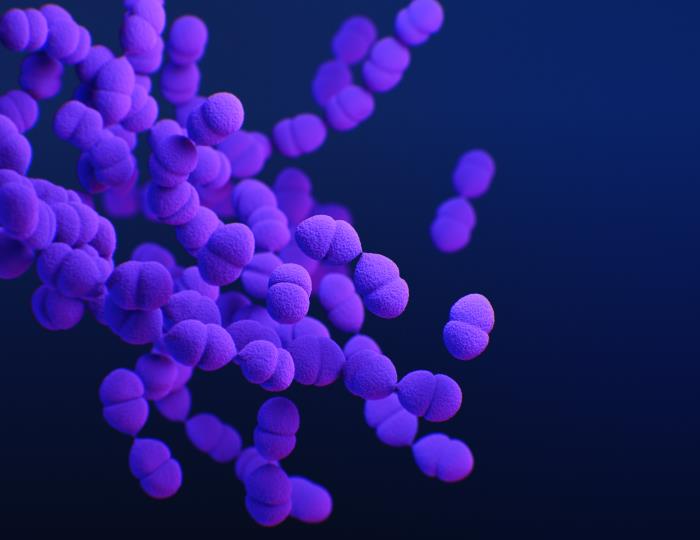
And those of us on the front lines of public health have also been keeping a close eye on increasing rates of group A Streptococcus (group A strep) in the United Kingdom and European countries.
Here's what you need to know on this common cause of "strep throat."
How do you get strep throat?: Watch out for these early signs of the highly contagious illness
More: What you need to know about RSV, the flu and virus myths
The ER or urgent care? How to know where to go when you get sick.
Cases of group A strep are higher than usual
Group A strep is the most common cause of bacterial pharyngitis – or "strep throat" in school-age children. Symptoms typically include sore throat, headache, fever and a fine red rash known as scarlet fever. The diagnosis is made with a rapid antigen test or bacterial culture, and treatment is with antibiotics and acetaminophen or ibuprofen for fever and pain.
Group A strep can sometimes lead to more severe, life-threatening disease known as invasive group A streptococcus (iGAS) and cause pneumonia, sepsis or infection of the skin and bones. A number of European countries started reporting an increase in cases of iGAS in children under 10 as early as September. The rate was many times higher than what was typically seen before the pandemic.
The CDC issued an alert on Dec. 22 about an increase in cases of iGAS in the U.S. It noted an increase in cases between September and November, above what was seen in previous years, but we don't have enough evidence to say that the rates are higher here in the U.S. than in pre-COVID years.
But given the experience of other countries, we should not be surprised if iGAS cases continue to increase nationally. Physicians and parents should remain vigilant.
I went to the ER, and things are not getting better. When is it time to go back?
Waking up with a stuffy nose?Why does this happen? And simple hacks to prevent it.
Is there a connection between the flu vaccine and strep throat? No.
This myth seems to have stemmed from a small study in mice that showed the nasal spray influenza vaccine led to an increase in group A strep colonization.
There are a few things wrong about this. While children under 2 in the U.K. are given the flu vaccine as a nasal spray, this vaccine spray is different from the one used in the study. Secondly, the presence of group A strep or other organisms does not mean infection.
The fact is that an infection with flu can lead to group strep A as a secondary bacterial infection. A more well-done pre-print study out of the United Kingdom showed that the nasal flu vaccine actually indirectly reduced rates of Strep A in children.
As such, it's important for everyone, including kids, to get the flu vaccine this year. Studies show the flu vaccine is a good match for the dominant H3N2 strain. The flu vaccine in general reduces the risk of flu illness by 40-60%.
Increases in strep are associated with increases in respiratory viruses
Scientists on both sides of the Atlantic agree that the increase in Group A strep and iGAS are associated with and a result of the surge in viral respiratory infections in children, such as RSV.
Viral interference from COVID-19 (and COVID-19 mitigation methods) kept other viruses at bay during the 2020 and 2021 winters. But that resulted in a large cohort of kids who were never exposed to these typical childhood viruses on a standard timeline. An earlier-than-usual outbreak of RSV and flu was the final ingredient in a perfect storm of viral infections. These viral infections predisposed kids to increased rates of group A strep.
However, this increase in cases is not due to a new strain of group A strep. And the common bacterial disease is not resistant to available antibiotics either.
What to know about preventing and treating strep throat
- Penicillin and amoxicillin are the mainstays of antibiotic treatment for uncomplicated group A strep. For those with a true penicillin allergy, clindamycin is also a great option.
- Early diagnosis of Group A strep and treatment with antibiotics is important because treatment can reduce further spread of the disease and prevent risk of complications like iGAS.
- Because Group A strep is the most common cause of bacterial pharyngitis in school-age children, it's crucial that schools emphasize good hand hygiene and indoor ventilation systems.
Group A Strep is increasing like other viral respiratory illness in children. Though it's not on the same level as countries in Europe, here in the U.S., we need to be vigilant to rapidly diagnose and treat infections to prevent complications such as iGAS.
More: Have you been told you're allergic to penicillin? Here's why you're probably not.
More: Common flu vaccine myths debunked: What you need to know this flu season
Michael Daignault, MD, is a board-certified ER doctor in Los Angeles. He studied Global Health at Georgetown University and has a Medical Degree from Ben-Gurion University. He completed his residency training in emergency medicine at Lincoln Medical Center in the South Bronx. He is also a former United States Peace Corps Volunteer. Find him on Instagram @dr.daignault
Comments
Post a Comment